How to Improve Rebate Management in a Hospital?

Managing pharmaceutical and medical rebates in healthcare organizations requires careful coordination across purchasing, claims, billing, and formulary operations. When these processes are not aligned, organizations risk missed revenue, higher drug costs, and unnecessary administrative burden.
Improving rebate management depends on strengthening three connected areas: rebate operations, claims adjudication, and therapeutic interchange programs. Together, these elements support lower net drug costs, stronger compliance, and smoother revenue cycles.
Table of Contents:
- Strengthen Core Rebate Management Processes
- Improve Claims Adjudication to Protect Rebate Revenue
- Use Real-Time Adjudication to Reduce Errors Early
- Apply Therapeutic Interchange Programs to Support Formularies
Jump to a section that interests you, or keep reading.
Strengthen Core Rebate Management Processes
Capturing drug manufacturer rebates allows healthcare organizations to reduce net drug costs and redirect resources toward quality care and financial stability. A key first step is understanding rebate eligibility.
Organizations must review agreements with group purchasing organizations, partner organizations, and payers before submitting rebate claims to avoid duplicate submissions. Eligibility review ensures claims are accurate and compliant from the outset.
Key Rebate Management Activities
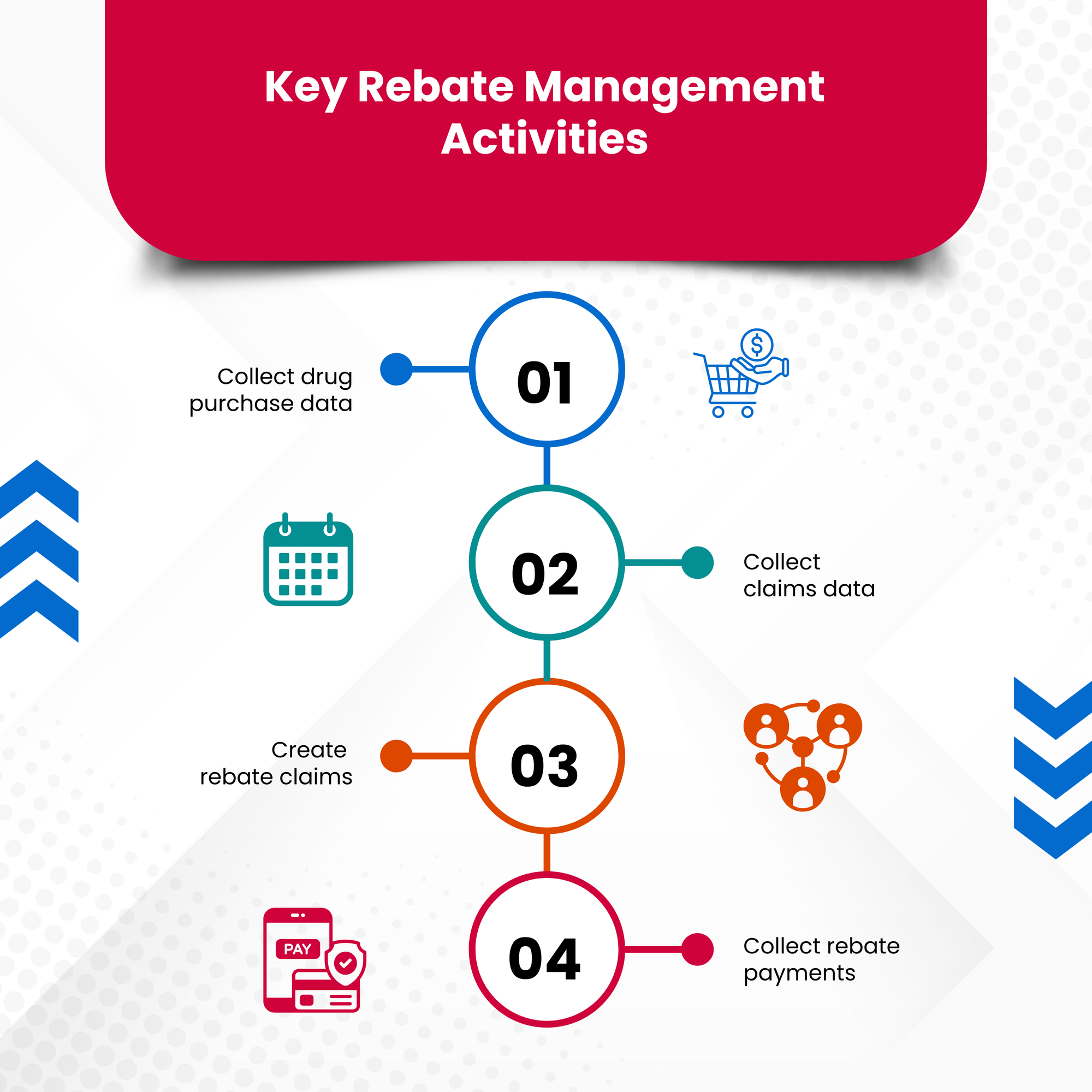
Improved rebate management relies on a structured workflow:
-
Collect drug purchase data: Monthly invoices contain details of all drugs purchased or billed. Reviewing this data helps identify rebate-eligible products and estimate potential rebate value.
-
Collect claims data: Medical rebates require claims data for administered drugs, while pharmaceutical rebates rely on claims to confirm treatments align with plan benefits and manufacturer rules.
-
Create rebate claims: Claims must be submitted in the required format with complete and accurate data to maintain access to manufacturer rebates.
-
Collect rebate payments: Rebates are commonly paid quarterly after claims are adjudicated to confirm accuracy and eliminate duplicates.
Pharmaceutical rebates can lower net drug costs by 5–10%, but the process is often time-intensive and depends heavily on claims accuracy. Manufacturer-specific submission requirements further increase complexity.
Many organizations partner with rebate management services such as Thirdwave RX to manage data ingestion, claim submission, and payment processing. Automating submissions and delivering rebates on a monthly basis reduces workload and improves cash flow consistency.
Improve Claims Adjudication to Protect Rebate Revenue
Claims adjudication ensures that submitted claims contain accurate, complete, and correctly formatted information. This step reduces workload across the reimbursement chain, including payers, PBMs, and manufacturers.
Organizations that do not adjudicate claims often experience higher denial rates due to errors or missing data. This leads to rework, appeals, delayed reimbursement, and potential revenue loss.
Common Errors Claims Adjudication Helps Prevent

- Incorrect ICD-10 or CPT codes
- Typos in patient or billing information
- Missing or incorrect patient details
- Bundling, downcoding, upcoding, and unbundling errors
- Incomplete patient records
- Duplicate claims
For larger healthcare organizations—such as health systems, long-term care operators, pharmacies, and specialty practices—adjudicating claims in-house supports operational efficiency and smoother revenue cycles.
When rebate claims rely on claims data, adjudication becomes even more critical. Ensuring correct formatting and identifying duplicates before submission reduces complications for manufacturers and protects future rebate access.
Use Real-Time Adjudication to Reduce Errors Early
Real-time adjudication platforms review claims before submission by pulling data from electronic health records and billing systems. This approach identifies errors and missing information earlier in the process and reduces staff workload.
By correcting issues upfront, organizations reduce denials, limit rework, and maintain cleaner data for rebate claims. Platforms capable of handling high claim volumes support consistent accuracy across large organizations.
Apply Therapeutic Interchange Programs to Support Formularies
Therapeutic interchange programs help enforce formulary decisions in complex healthcare settings. When off-formulary medications are prescribed, these programs allow organizations to substitute therapeutically equivalent drugs that align with formulary guidance or operational goals.
Implementing a therapeutic interchange program requires awareness of state regulations, clinical requirements, and business processes. These programs are customized to each organization and can only be used in specific states.
Therapeutic interchange programs are typically designed by pharmacy benefit managers and approved by clinical teams, as these groups oversee formulary decisions. Delegating this responsibility to teams already managing formulary or benefit design helps control costs linked to off-formulary prescribing.
Conclusion
Improving rebate management in healthcare organizations depends on tightening existing processes rather than adding complexity. Clear eligibility review, structured rebate workflows, accurate claims adjudication, and formulary enforcement through therapeutic interchange programs all contribute to lower net drug costs and steadier revenue.
When rebate management, claims accuracy, and formulary adherence work together, healthcare organizations are better positioned to reduce administrative strain while protecting both financial and clinical outcomes.
